
Blog
want to take a crack at your problems from home? Check out our blog posts and find the topics specific to you
Topics:
Unleashing the Power of Intrinsic Foot Strength in Endurance Running
In the world of running, where every stride adds up and the body keeps score, the significance of intrinsic foot strength often goes unnoticed until it can’t be ignored. While many runners focus extensively on building leg strength, improving cardiovascular endurance, and perfecting their running form, the role of the feet tends to be overlooked. However, understanding and harnessing the power of intrinsic foot strength can be a game-changer for endurance athletes, enabling them to run longer, faster, and with reduced risk of injury.
Introduction:
In the world of running, where every stride adds up and the body keeps score, the significance of intrinsic foot strength often goes unnoticed until it can’t be ignored. While many runners focus extensively on building leg strength, improving cardiovascular endurance, and perfecting their running form, the role of the feet tends to be overlooked. However, understanding and harnessing the power of intrinsic foot strength can be a game-changer for endurance athletes, enabling them to run longer, faster, and with reduced risk of injury.
What is Intrinsic Foot Strength?
Intrinsic foot strength refers to the strength and stability of the muscles within the foot itself. These muscles play a crucial role in maintaining proper foot mechanics, providing support, absorbing shock, and facilitating efficient propulsion during running.
Why is it Important for Endurance Runners?
Endurance running places significant demands on the feet, as they repeatedly absorb the impact of each stride over long distances. Weakness or instability in the intrinsic foot muscles can lead to various pain patterns, including plantar fasciitis, shin splints, and bone stress injuries. By developing strong and resilient feet, endurance runners can enhance their performance while reducing the risk of common overuse injuries.
Benefits of Strong Intrinsic Foot Muscles:
1. Enhanced Stability: Strong intrinsic foot muscles contribute to better foot stability, allowing runners to maintain proper alignment and balance, especially on uneven terrain.
2. Improved Propulsion: A strong arch provides a solid platform for pushing off the ground with greater force, resulting in more powerful strides and increased speed.
3. Injury Prevention: By distributing forces more evenly throughout the foot, strong intrinsic muscles help reduce the risk of overuse injuries caused by excessive stress on specific areas.
4. Efficient Energy Transfer: Proper foot mechanics supported by strong intrinsic muscles optimize energy transfer from the ground to forward motion, conserving energy and delaying fatigue during long runs.
How to Develop Intrinsic Foot Strength:
1. Barefoot Exercises: Performing exercises barefoot, such as toe scrunches, arch lifts, and towel curls, can target and strengthen the intrinsic foot muscles.
2. Minimalist Footwear: Transitioning to minimalist or barefoot-style shoes encourages natural foot movement and strengthens the muscles by providing less cushioning and support.
3. Foot Strengthening Tools: Using tools like resistance bands, balance boards, or specialized foot strengthening devices can further challenge the muscles and improve their strength and endurance.
4. Gradual Progression: It's essential to progress gradually when training the intrinsic foot muscles to avoid overuse injuries. Start with low-intensity exercises and gradually increase the duration and intensity over time.
Incorporating Intrinsic Foot Training into Your Routine:
Integrating exercises to strengthen intrinsic foot muscles into your regular training regimen can significantly benefit endurance runners. Whether you're a seasoned athlete or just starting your running journey, prioritizing foot strength can lead to better performance, fewer injuries, and a more enjoyable running season.
Conclusion:
Building strong intrinsic foot muscles is not only essential for injury prevention but also for maximizing performance potential. By paying attention to the foundation of their stride, runners can unlock new levels of strength, endurance, and resilience on the road or trail. So, lace up your shoes, strengthen those feet, and embrace the transformative power of intrinsic foot strength in your endurance running journey.
Get Back Out There!
-Dr. Sam
How long does it take for Achilles tendonitis to heal? (updated 2024!)
Achilles Tendon pain can be super frustrating. Learn how long it might take you to recover
Achilles Tendon pain can be INCREDIBLY frustrating.
This is especially true if you can’t participate in your activities of choice because of the pain. I often see Achilles Tendinopathy in runners, hikers, volleyball players… It sucks for everyone.
The most common question I get when someone comes in with Achilles Tendon pain is “how long is this going to take”?
This is not my favourite question to answer, because Achilles Tendon pain can last a LONG TIME.
The short answer to that question is “1-12 months”, but that doesn’t really help anyone. The slightly longer answer to that question is “it depends”, which ALSO is not very helpful…
In order to estimate your recovery time, you need to understand two things:
Severity and Stage of your injury
Other factors that influence your performance
Let’s break it down a little bit, and you can see where you might fall in the estimated recovery time.
Grading the Severity and Stage of your Injury
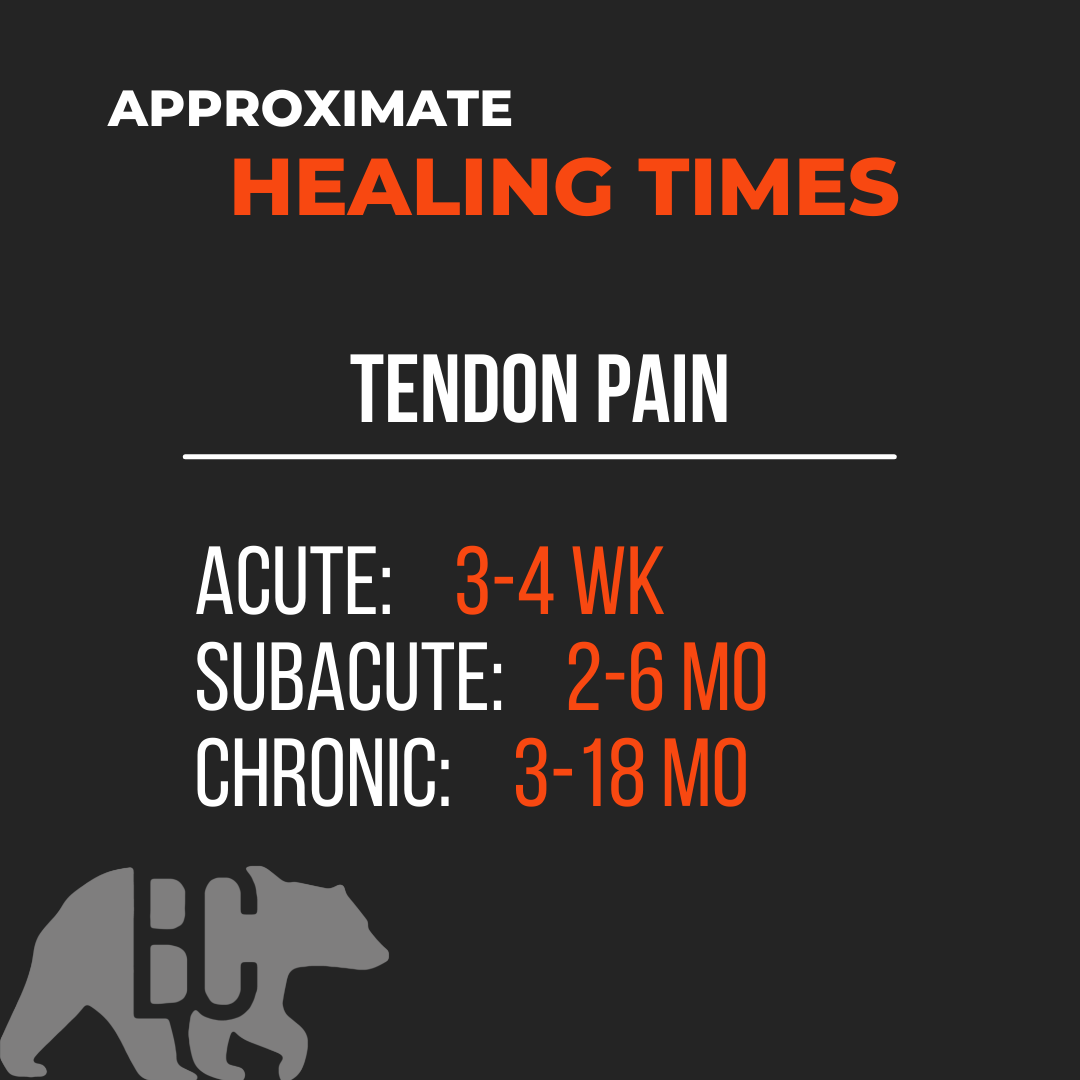
Achilles Tendinopathy falls into 3 Stages:
Acute (new onset of pain, up to 2 weeks)
Subacute (immediately after acute, 3 weeks-2 months
Chronic (3 months plus)
The later longer it has been since the onset of injury, the longer it generally takes to recover.
Acute Achilles Tendinitis will usually calm down in 3-4 weeks (I say CALM DOWN, not GET BETTER here. This is explained later in this article under the header ‘Calmed Down vs Gotten Better).
Subacute Achilles Tendinopathy will usually take 2-6 months to calm down. (Again, not better yet)
Chronic Achilles Tendinopathy is a tricky one and can take anywhere from 3 months to 18 months to calm down and get better.
FACTORS THAT INFLUENCE RECOVERY TIME
This list is a long one, so I will only list the ones I feel are most important. These include:
Overall Health
Crappy Diet? Super stressed out? Smoker? Comorbidities like diabetes, metabolic syndrome or heart disease? All of these things lengthen the expected recovery time.
Mindset
Positive mindsets win the rehab game.
Sleep
You can’t out rehab 5hrs per night of sleep, especially while trying to recover from an injury. You NEED 8hrs + of sleep per night if you want to get better in a reasonable time and keep the injury from coming back.
Rehab Plan
Your rehab plan needs to be well-thought-out, progressive, and appropriate to both your current state and the activities you want to get back to. If you are a runner and your rehab plan does not involve running at some point, you are following the wrong plan. Volleyball? You better be jumping at some point in your plan. (But not too much too soon…)
Calm Down vs Get Better
This happens time and time again. Someone comes to see me and together we are able to get them out of pain, and they feel better, so they decide to cancel their follow up and get back to their activity.
Inevitably, a couple of weeks later they are back in my office, 2-steps back.
This is because their injury was not fully rehabbed. Only their PAIN is better, but they have not been fully prepared to get back into their activity at 100%. This takes time, deliberate effort, and a well-thought-out progressive rehab plan.
Moral of the story: just because the pain goes away, does not mean that you are ‘better’ (especially true with Tendon injuries).
Rehab programs should generally have 3 Steps.
Step 1: Calm Stuff Down
Step 2: Build Back Up
Step 3: Bridge the Gap
MOST rehab plans end after calming stuff down. SOME plans do a decent job of building strength and endurance back up. VERY FEW programs bridge the gap between recovering from an injury and performing the way you want to.
Need some help?
That is where we come in. If you are ready to get on a plan that will get you back in action and back to doing the things you love, and KEEP THIS INJURY FROM COMING BACK, we can help.
Author: Dr Mark Murdoch, Chiropractor and Co-Founder at Base Camp Sport and Spine in Vernon, BC.
Mark Murdoch is a Doctor of Chiropractic with a Master’s Degree in Sports Medicine.
Contact: drmurdoch@basecampclinic.com
Book an Appointment with Dr Murdoch: book here
Instagram: Base.Camp.Doc
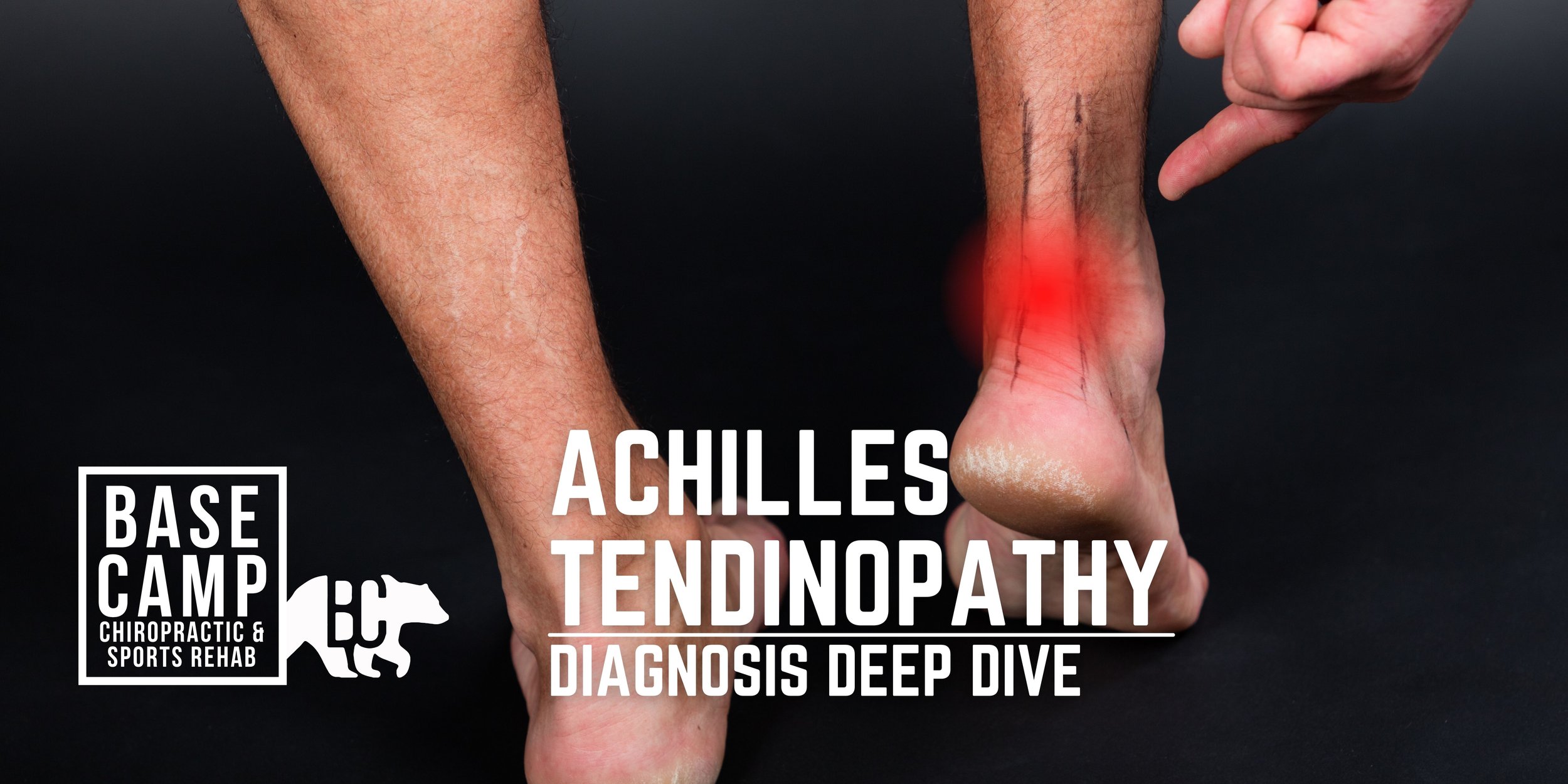
Achilles Tendinopathy (UPDATED 2024!)
One of the most common running injuries, Achilles tendon pain can sideline you for months. If you think you might have Achilles tendinopahty, make an appointment today so we can get you back to doing what you love.
In this article:
what is Achilles tendinopathy
Who gets Achilles tendinopathy
How we diagnose Achilles tendinopathy
What to do if you have Achilles tendinopathy
It goes a little something like this…
You’re new to running and decided that trail running is for you (YES! Stoked for you). The runs so far have been pretty enjoyable, but you are ready for something a little bit more challenging than the Rail Trail. This week you are ready to put some miles in at Kal Park! Can’t be that hard right?
So you pick up a brand new pair of Trail Runners, pick a trail and start moving.
It went great! You had such a blast. The VIEWS! They were just amazing. Sure, the hills were hard, but that’s good for you, right? Nothing like a little uphill challenge.
The next couple of weeks go great. Instead of road running, you are strictly on the trail and instead of the measly Rail Trail, you are strictly running the rolling hills of the North Okanagan.
One day while running your new favourite Kal Lake route you start to feel some discomfort in your lower leg. It’s on the backside, a couple of inches up from your heel. That’s weird. This has never happened before. It’s not a big deal though. After a km or so it goes away and for the rest of the run you don’t even feel it. “It must have been nothing”, you think.
But the trend continues… next week you are feeling the same pain on every run and it’s starting to last longer. It doesn’t quite go away by the end of your run. Instead, it keeps getting worse! After your run it calms down, but lingers for a few hours. “This must just be part of becoming a runner. I just have to deal with some pain sometimes”.
The next morning you step out of bed and OUCH. Your Achilles HURTS! It’s a tension/burning/shearing pain. It hurts to stand and it hurts to walk.
What the heck is going on?
ANSWER:
A good ol’ case of Achilles Tendinopathy.
What is it?
Achilles Tendinopathy is a really common overuse running injury. As many as 85% of middle-distance runners will experience it.
The Achilles is a tendon that attaches your calf muscle (back of your lower leg) to your foot. It attaches to the top of the back of your heel and is one of the main ways we transfer force through our feet while running and walking. When we start to get Achilles pain it can start to affect EVERYTHING YOU DO throughout your day. It sucks, but most people recover from it with proper treatment and rehab.
Tendinopathy is a fancy word to describe an inflammatory and remodelling response process that happens when the Achilles tendon is overloaded and is unable to recover. The catch is that it will often get worse if it is just ignored. Early recognition and intervention are key in shortening the recovery time.
A typical case of Achilles tendinopathy starts slow and becomes more severe over time until it is present every time the tendon is loaded.
Who gets it?
While Achilles Tendinopathy seems like it should be more prevalent in competitive athletes, 65% of cases are from the general public and are not sport-related.
There are a few risk factors that increase your chance of getting Achilles Tendinopathy that I divide into 2 categories: things you CAN control and things you CANNOT control
Things you CAN control:
Ankle strength (weak ankles, especially with pressing your toes down, is a risk factor)
Sudden changes in training volume (too much, too soon)
Uphill running (if you are unprepared for it)
Fluoroquinolone antibiotic use (e.g. ciprofloxacin) has been shown to significantly increase the risk of tendon injuries (not just Achilles tendon!). If you are on antibiotics, it is wise to change your training program temporarily. Talk to your prescribing doctor if you are unsure about the type of antibiotics you are taking and if there are alternatives
***Increased body weight and abnormal ankle range of motion. While these aren’t always completely within our control, a little change can go a long way. You don’t need to have perfect range of motion or body composition to avoid Achilles tendinopathy
Things you CANNOT control:
Family history of tendon injuries
Genetic variation
Systemic disease
Abnormal ankle range of motion.** (If you have a previous injury that limits your range of motion or have hypermobility, your ROM might be out of your control).
How does a doctor diagnose Achilles tendinopathy?
As a Chiropractor in Vernon, BC, who sees a lot of sports-related injuries, I use a two-stage process to diagnose Achilles Tendinopathy
Step 1: History
During the history portion, I ask a ton of questions to determine if Achilles tendinopathy is responsible for your symptoms.
There are some typical things we hear in the history that tip me off as a Sports Medicine practitioner:
Pain at the Achilles tendon, either in the middle of the tendon, the heel, or the tendon-muscle junction
Pain that has progressed over time and gotten worse with activity
Engaging in a running, walking, or pedalling activity
Previous history of tendon pain or injury
Other aspects of a patient history I look for when a patient comes in with Achilles pain:
Antibiotic use (certain antibiotics increase the risk of tendon injuries)
Recent increases in training volume
Changes in training terrain (especially adding hills to a running program)
Changes in running footwear
Family history of tendon injuries
Systemic diseases
Other life stressors
Step 2: Physical Exam
During the physical exam, I test out your joints, muscles and tendons, check your range of motion, and strength, and perform some other tests to determine the cause of your pain, the severity of your injury, and your current limitations.
Here are some things I typically look for on a physical exam for Achilles tendinopathy:
Pain with pressure (usually a pinch) on the Achilles Tendon
Pain with loading the tendon (pressing your foot down, like a Calf Raise)
Thickening of the tendon or nodules on the tendon
Redness or swelling along the tendon
Endurance of the calf musculature
Ankle, knee, and hip range of motion
Strength of the ankle and knee
Check your gait (running and walking)
What to do when you have it?
One of the most important things to do if suspect tendinopathy is to NOT WAIT to get an assessment, get treatment, or change your training. The worse a tendinopathy gets, the longer it can take to heal.
Here is what the typical process looks like:
STEP 1: Get Assessed.
STEP 2: Get A Plan.
STEP 3: Get Better.
Achilles tendinopathy does not always mean you need to completely stop your activity, but a period of relative rest is essential. In order to heal we need to decrease the demands on the tendon to a level that you can recover from.
If you suspect you have Achilles tendinopathy, take a couple of days off of your primary activity (for this example we will use running) and see how your body responds. If you notice your pain is going down, it is wise to take a week or two off and then try a short slow run.
In my treatment room, the first thing I use to treat Achilles pain is a combination of manual therapy and exercise to manage pain. Once the symptoms start to calm down, we start building your strength and endurance back up. After a period of strength training, we slowly build back up to running.
How to treat your Achilles Tendinopathy from home:
**NOTE: Achilles tendinopathy is not something I recommend most patients manage by themselves. Having a clinician to help guide you improve your chance of success and decreases your chance of re-aggravation.
Treatment follows 3 Steps: 1) Calm it Down, 2) Build if Back Up, 3) Get Back to Activity
Phase 1: Calm it Down
ISOMETRICS (Weeks 1-2)
The first thing we want to do is manage your symptoms. This is especially important if you have any swelling.
Relative Rest/Deload: take 2-3 days off of your activity and see how you respond. If you are worried about your running fitness, try switching it up for cycling, rowing, swimming, or circuit work that does not include running or skipping
Self-Myofascial Work/Foam rolling: this can give some temporary relief for the calf and ankle. Avoid rolling out directly on top of the painful tendon
Isometrics: isometrics are exercises that load the muscle and the tendon but simultaneously provide a pain-relieving effect. I typically recommend my Achilles tendon patients use some variation of this home exercise prescription:
Phase 2: Build it Back Up
The next phase of Achilles tendinopathy rehab is to build your strength and endurance back up. I use eccentric exercises first and then progress into concentric exercises.
ECCENTRICS (Weeks 2-5)
Eccentrics allow us to load the calf and its tendon in a way that is highly controlled. The key to using Eccentrics here is tempo, and not moving too quickly throughout the exercise.
At the start of Week 3, if symptoms have calmed down, re-introduce a short, slow run just to gauge how your recovery is going. When I say short I mean SHORT. 400-1000 m is enough. If you tolerated it well (mild pain during the run, and lingering pain that does not last more than 24 hours) then you can start running that distance ONCE per week.
FULL RANGE OF MOTION (Weeks 6-9)
Using the full range of motion of the ankle puts the muscle through each type of contraction. The only reason I use concentric exercise AFTER eccentric exercise is that for many patients it is easier to control in this order.
We progress each exercise from both feet to one foot as tolerated to prepare the tendon to handle your full body weight.
At the start of Week 5, re-introduce up to 30% of your typical running distance for the next two weeks (e.g. if you run 10km in a week, limit yourself to 3km for Weeks 5 and 6)
At the start of Week 7, re-introduce up to 50% of your typical running distance for the next two weeks (e.g. if you run 10km in a week, limit yourself to 5km for Weeks 7 and 8)
Phase 3: Get Back to Activity
This is where we start to risk re-aggravation. While some pain is normal and acceptable with tendon rehab, we don’t want to go backwards, but we also want to push your limitations so that we know you are closer to getting back to your activity at as close to 100% as possible.
BALLISTICS (Weeks 10-12)
Ballistic exercises (hopping, skipping, running, etc.) load the tendon rapidly and take advantage of its elastic properties (one of the main functions of the tendon). The tricky part here is that it is the elastic nature of the tendon that causes the damage in the first place (the elastic was overstretched too many times before it could heal). This is why a gradual introduction of ballistic exercise is essential. It is best to progress slowly.
How long does it take to recover?
I would like to apologize in advance for this next part. Firstly, because you are not going to like and answer, and secondly because there really ISN’T a concrete answer.
Like most injuries, Achilles tendinopathy recovery varies from person to person, but if left untreated it can take UP TO A YEAR to recover. Oof.
That said, not everyone will take so long to recover. How quickly you recover will depend on a few things such as:
How quickly you recognize there is a problem and change what you are doing. Early recognition and then intervention leads to faster recovery because we can start treatment and rehab BEFORE the injury becomes severe.
Have you had tendinopathy in the past? This may take longer to heal
Are you currently on antibiotics? This one is a tricky one (caveat: I am not a medical doctor, and you should always consult your prescribing doctor before messing with your medication), but sometimes can be super simple. In some cases, simply finishing your antibiotics course or changing antibiotics is all it takes.
Do you have optimal ankle ROM? If you have limited range of motion, work to improve it. If you have excess range of motion, work on ankle strengthening
What is your overall health? Stress level? Improving other areas of your life can improve your ability to heal from injury.
Should I stop running?
Ahhh, here we go. The real reason you are here. Should I stop running with Achilles tendinopathy? This is, again, a super complex question. Kind of like “should I buy a house?” or “should I get face a tattoo?”. There are going to be different answers for every person who asks the question, and context is essential to making the right decision.
In many cases of Achilles tendinopathy, a period of relative rest IS essential to the healing process. Unlike other injuries, tendinopathy is hard to work around and keep running.
That said, there are some strategies to keep you running. If you need to keep running, here are some modifications that can be helpful:
Avoid uphill running
For a period of time, shorten your runs. Start with 50% of your normal distance and see how you feel.
Find a shoe with a higher drop (the difference between your heel and your forefoot). This can help take some of the stress off your Achilles while you are rehabbing.
GET ON IT EARLY. The earlier you recognize you may have Achilles tendinopathy the better your chances of a quick recovery.
Start rehab and see how you feel. I try and keep as many of my patients running as possible, even while they continue to rehab their Achilles
How to avoid it
Simple. All you need to do is manage all of the stressors in your life, get enough sleep, and never train more than you can recover from, and eat a perfect diet.
Ok… maybe not as easy as it sounds.
Unfortunately, controlling all of the variables involved in order to avoid Achilles Tendinopathy is not always possible. BUT there are at least a few things you can do.
IMPORTANT NOTE: just because you can’t do ALL of these tips, does not mean that doing SOME of them is not helpful. Pick one or two and focus on getting them right, then add in the others later.
SLEEP
Aim for 8+ hours of sleep per night. There is NOTHING more protective from injury than sleep.
NUTRITION
Get enough protein (1.1-2.5 grams of protein per kg of body weight per day) from as many whole sources (animal sources) as possible. Getting enough can be hard, so don’t be afraid to supplement with a protein shake if needed.
STRENGTH
Resistance train (lift weights) 1-3 times per week. Specifically for Achilles pain, heavy calf raises with your knee straight and again with your knee bent is really helpful.
MANAGE YOUR STRESS
If you are mega stressed out, your injury risk goes up. Consider using mediation, yoga, breathwork, or other relaxing methods to manage your stress.
MANAGE YOUR TRAINING
Too much, too soon. If you are new to running, don’t be afraid to take it slow. This recommendation is doubly relevant if you aren’t managing any of the other aspects of injury.
GET CHECKED
Think you might have Achilles Tendinopathy? Get checked. Don’t let it get so bad that you have to sideline your training.
Author: Dr Mark Murdoch, Chiropractor and Co-Founder at Base Camp Chiropractic and Sports Rehab in Vernon, BC.
Mark Murdoch is a Doctor of Chiropractic with a Master’s Degree in Sports Medicine.
Contact: drmurdoch@basecampclinic.com
Instagram: Base.Camp.Doc
Disclaimer: This blog is intended for general informational purposes only and is not intended for the delivery of medical advice. No doctor/patient relationship is formed. The use of information on this blog or materials linked from this blog is at the user's own risk. The content of this blog and website is not intended to be a substitute for medical advice.















How running injuries happen